Arthroscopic Rotator Cuff Surgery
Rotator cuff tears are a common source of shoulder pain in adults. They are frequently injuries from wear, rather than trauma. Our busy lives and everyday activities take their toll on these tendons over time. Consequently, as our bodies age, we become more prone to wear-type injuries. If you are suffering from shoulder pain, a rotator cuff tear could be the problem.
The pain from a rotator cuff tear may develop suddenly or gradually—in the beginning it may be noticed only with overhead activities such as reaching or lifting. At first, you could find relief by resting your shoulder or taking Motrin or aspirin. Over time, however, the pain can become noticeable even when you rest. You may also experience stiffness and loss of motion. These tears are often seen in individuals who perform frequent overhead activities such as construction work or painting. Certain athletes, such as swimmers, pitchers and tennis players also seem to be at increased risk. Unlike the slow progression of the wear injury, when the tear occurs traumatically there may be sudden acute pain, a snapping sensation, or even an immediate weakness of the arm.
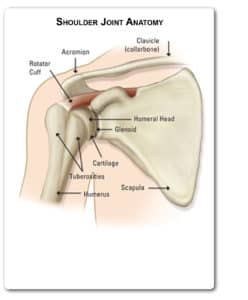
The rotator cuff itself is an intricate part of the complex shoulder anatomy that allows the shoulder to move in many directions. It is made up of four tendons—supraspinatus, infraspinatus, teres minor, and subscapularis—and their muscle units. These tendons combine to form a “cuff” over the upper end of the arm. The muscles originate from the shoulder blade and form a single tendon that helps to lift and rotate the arm and to stabilize the ball of the shoulder within the joint.
An orthopaedic surgeon can help you determine if you might have a rotator cuff tear based on a combination of your symptoms, examination, and special tests. During the exam, the doctor will look at your shoulder for areas of tenderness or see if there is a deformity. He or she will also measure the range of motion of your shoulder in several different directions and test the strength of the arm. The doctor may also examine your neck to make sure that your pain is not coming from a pinched nerve in your cervical spine and to rule out other conditions such as arthritis.
Diagnosis
Common tests used in diagnosing a rotator cuff tear include X-ray and MRI. A X-ray of a shoulder with a rotator cuff tear is usually normal or may show a small spur. For this reason, the doctor may also order an additional test called a MRI (magnetic resonance imaging). This test better visualizes soft tissue structures such as the rotator cuff tendons. A MRI can also help to distinguish between a full thickness (complete) tear of the tendon and a partial tear. It can show the doctor where the tear is located and how much of the cuff is involved. Once a diagnosis of rotator cuff tear has been made, the surgeon will recommend the most effective treatment.
Treatment
Treatment for a rotator cuff tear can be operative or non-operative. In many instances non-surgical treatment can provide pain relief and can improve the function of your shoulder. Non-operative treatment may include rest and limited overhead activity, use of a sling, anti-inflammatory medications such as Motrin or Aleve, steroid injections, and/or physical therapy.
Surgical management is recommended for rotator cuff tears that do not respond to conservative management and/or are associated with weakness, loss of function, and limited motion. Surgery may also be considered if the tear is acute and painful, if it is the dominant arm of an active individual, or if you need maximum strength in your arm for overhead work or sports.
The choice of surgical technique depends upon several factors including the orthopaedic surgeon’s experience and familiarity with a particular procedure, the size of the tear, patient anatomy, quality of the patient’s bone and tendon tissue, and the patient’s needs. Regardless of the repair method used (Body Wise Vol.3, No.2), each repair type shows similar levels of pain relief, strength improvement, and patient satisfaction. Many surgical repairs can be done on an outpatient basis.
Surgery
Arthroscopic surgery is both a diagnostic and surgical procedure. It is often recommended for patients who did not respond well to initial conservative treatment. This technique allows the surgeon to evaluate the shoulder joint from inside the joint using a tiny camera and surgical tools passed through small incisions (termed portals). It is a useful diagnostic technique; and fortunately, due to increasing advances in the field of arthroscopy, most treatments and repairs can also be performed at the same time as the initial arthroscopic evaluation. Through the use of additional portals the orthopaedic surgeon may complete the entire surgical procedure arthroscopically.
Shoulder impingement and rotator cuff tears are common conditions that are frequently treated with arthroscopic surgery. During arthroscopic treatment, worn, torn, or inflamed tissues are trimmed or “smoothed out” to help restore the joint mechanics and help promote healing. In addition to smoothing and shaving the bone, the orthopaedic surgeon may also remove any loose tissue found in the joint. If the source of the patient’s shoulder pain however, is secondary to a tear, more extensive arthroscopic surgery is then indicated. Operative treatment of a completely torn rotator tendon is designed to repair the tendon back to the humeral head (ball of joint) from where it is torn. This can be accomplished in a number of ways. Each of the methods available has its own pros and cons, but all have the same goal–getting the tendon to heal to the bone. The overall complication rate following rotator cuff surgery is estimated to be about 10 percent. The most frequent complication is tendon retearing, followed by joint stiffness, deltoid detachment (which can be avoided by arthroscopic techniques), nerve injury, and infection.
Regardless of which procedure is performed, the arm is immoblized after surgery to allow the tear to heal. Therapy then progresses in stages. Initially, the repair needs to be protected until adequate healing of the tendon to bone occurs. For this reason, most patients use a sling for the first four to six weeks after surgery and are instructed to limit active use of the arm during this period. Passive range-of-motion exercises are begun with a therapist. Progressive strengthening and range of motion exercises continue during the next six to 12 weeks. Most patients have a functional range of motion and adequate strength by four to six months after surgery. A strong commitment to rehabilitation is important to achieve a good surgical outcome. The doctor will advise you when it is safe to return to overhead work and sports activity.
In summary, rotator cuff tears can be a source of pain in the shoulder and their incidence increases with patient age. Initial treatment is often non-operative and can result in decreased pain and improvements in range of motion; however, a completely torn tendon will not recover in this fashion and strength may not be restored. Arthroscopic surgical repair is often a good option for patients with residual symptoms and can result in improved function and strength in more than 80 percent of patients.

Dr. Rocca is Board Certified in Orthopaedic Surgery and has completed Academy subspecialty certification in Sports Medicine. Prior to joining The Orthopaedic Insitute, he practiced eleven years with the United States Navy. Dr. Rocca attended medical school at the University of Pennsylvania and completed his residency in Orthopaedic Surgery at the National Naval Medical Center. He also performed a fellowship in Hyperbaric Medicine at the Naval Undersea Medical Institute. Dr. Rocca is a member of the American Academy of Orthopaedic Surgeons, Florida Orthopaedic Society and Florida Medical Society.

