Low Back Pain’s Missing Link: Diagnosing the Sacroiliac Joint
About 85 percent of all people will have lower back pain at some point in their life. Low back pain is second only to upper respiratory problems as a reason for visits to a physician or hospital, generating about 15 million visits a year. It is the fifth ranked cause of admission to the hospital and third most common cause of surgical procedures. In 2005, annual direct and indirect costs for treatment of low back pain reached about $86 billion.
According to published scientific literature, up to 30 percent of all low back symptoms are sacroiliac joint in origin, but the diagnosis of a problem with the sacroiliac joint is frequently overlooked because low back pain symptoms have many causes as well as hip joint symptoms. In fact, many patients with disabling low back pain issues go on to receive lumbar spinal treatments and/or hip treatments. Although the source of their symptoms may be sacroiliac joint in origin, either in whole or in part, leaving these patients with little or, in some cases, no relief.
What is the sacroiliac joint?
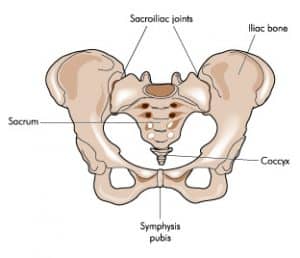
The sacroiliac joint forms the lowest segment of the spine, joining the sacrum to the pelvis. It distributes force delivered from the upper body. Sacroiliac joints are located on either side of the sacrum.
The function of the sacroiliac joint is to transfer weight and forces due to movement from the upper body, through the pelvis and to the legs, and vice versa. The pelvis acts as the central base through which large forces are transferred and dissipated. The primary role of the sacroiliac joint is to provide stability for the pelvis and to bear the load of the upper body.
Why does the sacroiliac joint cause problems?
Potential causes for the sacroiliac joint problems include degenerative disease, history of trauma, pregnancy, childbirth and after long-arm lumbar fusions where the forces are transmitted from the lumbar spine to the sacrum and, therefore, to the sacroiliac joint. The sacroiliac joint may be disrupted due to lack of joint continuity or suffer from sacroilitis.
The sacroiliac joint is a synovial joint, the most common movable type of joint. It has a nerve supply that originates from multiple lumbosacral root levels with partial innervation from L2 to S3 of the spine. Strong ligaments encase each joint and allow approximately two to four millimeters of movement during weight bearing and forward flexion. When these ligaments become damaged, either by normal wear and tear or by injury, they may have excessive motion. The excessive motion may inflame and disrupt the joint and surrounding nerves. When this happens, people can feel pain in their back or buttocks, especially with lifting, running or even walking. It is commonly reported in the clinical literature that up to 25 percent of all low back pain is caused by the sacroiliac joint. In addition, the incident of sacroiliac joint degeneration in post-lumbar fusion patients is 75 percent at five years post-surgery.
For many people who have low back pain associated with the sacroiliac joint, the pain begins spontaneously. However, in just as many reported cases, sacroiliac joint pathology can be related to a specific event, often an injury. It is difficult to directly relate any specific functioning difficulty including walking, sitting, standing, sleeping on the affected side, job activity, bowel movements, coughing, sneezing, etc., to the sacroiliac joint as a source of pain. One key indication is specific location of pain in the lowest back and buttock region.
Who is at risk for sacroiliac joint problems?
Injury from accidents including falls is a predisposing factor for sacroiliac joint pain. Women may be at increased risk for sacroiliac joint problems because of having broader pelvises, greater curve of the neck and shorter limb lengths. Pregnancy often leads to stretching the pelvis, especially in the sacroiliac ligaments.

Most published differential diagnoses for low back pain fail to consider the sacroiliac joint as the source of lower back pain, underscoring the need for proper diagnosis. The fact that the pain caused by sacroiliac joint dysfunction can mimic diskogenic or radicular low back pain, potentially leads to the wrong diagnosis and treatment, such as with lumbar spine surgery.
Sacroiliac Joint Symptoms and Diagnostic Methods
A variety of tests performed during a physical exam may help reveal the sacroiliac joint as the cause of low back pain symptoms. Point-specific pain, compression tests of the pelvis, distraction tests, and thigh thrust examination all can help aid the clinical diagnosis of sacroiliac joint dysfunction. In addition, X-rays, CT scan or an MRI may be helpful in diagnosis. However, the most relied-upon method to accurately determine whether the sacroiliac joint is the cause of low back symptoms is to inject the sacroiliac joint with a local anesthetic. This injection can be diagnostic as well as therapeutic. The injection is delivered with either fluoroscopic or CT guidance to verify accurate placement of the needle in the sacroiliac joint. If symptoms are significantly decreased, it can be concluded that the sacroiliac joint is either the source or a major contributor to low back symptoms. Physical therapy is certainly part of the treatment paradigm for sacroiliac joint dysfunction.
iFuse SI Joint Fusion Procedure
The sacroiliac joint fusion with the iFuse Implant System is considered after failed conservative treatment. This is a minimally-invasive surgical treatment that stabilizes the sacroiliac joint by surgically inserting three titanium implants across the sacroiliac joint. This can be achieved through a 1.5 inch incision in the superior gluteal region. Under fluoroscopic guidance and minimally-invasive techniques, three triangular titanium implants can be inserted across the sacroiliac joint itself.
Potential benefits of the minimally-invasive iFuse procedure:
- Less invasive than traditional open surgery.
- No extensive soft tissue stripping.
- Minimal incision size.
- Minimal tendon irritation.
- Reduced risk of infection due to small surgical incision and reduced operative time.
- Decreased length of stay; all patients stay in the hospital overnight and are discharged the following day.
The iFuse procedure typically takes 1 hour and requires an overnight hospital stay. The procedure can be done using either local or general anesthesia; the surgeon will determine the most appropriate method based on the patient’s overall condition.
The iFuse Implant System is intended for sacroiliac joint fusion for conditions including sacroiliac joint disruptions and degenerative sacroilitis.

Dr. Stevenson is board certified in neurosurgery. He attended medical school at the University of Glasgow and completed his residency in neurosurgery at Duke University Medical Center. Dr. Stevenson is a fellow of the Royal College of Surgeons in England. He is a member of The American Association of Neurological Surgeons, the Congress of Neurological Surgeons and The American College of Spine Surgery. When he is not working, Dr. Stevenson enjoys spending time with his family.

